
Bed Stay – Immobility and HA DVT
The risk for DVT in active adults is .001%. Every step taken activates calf muscle contractions, promotes venous outflow towards the heart, and prevents DVT.
Once hospitalized, immobility sets in and the rate for DVT increases 4,000 times to 3-5% or higher.
Hospital bed stay leads to calf muscle pump failure and a significant reduction in venous outflow, which increases the risk for DVT. Up to 10% of hospital deaths are attributed to DVT.

Bed stay increases risk for DVT.
Patients undergoing joint replacement surgery are assessed for inherent risk factors for developing DVT and the probability of developing DVT at a rate of 6.5% – 18%. SCDs are not provided for use during home recovery which exposes high-risk patients and hospitals to unwanted readmissions due to DVT.
For high-risk patients, the need for DVT Prevention Therapy is elevated until returning to an active lifestyle.
Hospitals have been using bed-mounted sequential compression devices (SCDs) for over 40 years to help prevent DVT. Technology has changed little other than going from weighing 12 pounds to now 6-8 pounds. SCDs still do not promote ambulation. Patient compliance with SCDs is < 50%. Due to bulky size and high cost to replace if damaged, hospitals do not provide SCDs to high-risk patients during home recovery, which leads to delayed discharges, unwanted DVTs, and costly readmissions.
Nurses and Patients are frustrated with SCDs for the following reasons:
High Importance: Fail to promote ambulation. Hassle to remove and reapply SCD sleeves every time patient leaves the bed. Patient discomfort with heat buildup due to non-breathable limb sleeves. Constant pump noise disturbs rest and sleep, leading to patient compliance below 50%. Tissue pressure injuries developing due to SCD tubing rubbing against the skin (3.1%) further penalizes hospitals and patients with longer hospital stay requiring wound care treatments.
Moderate Importance: Inconsistent pump reliability, difficulty with attaching hoses, sleeves, and power cords, and issues involving patients and nurses tripping over hanging hoses and/or sleeves.



Fact: Those $6.00 SCD sleeves are costing hospitals millions each year!
- SCDs do not promote ambulation which increases the risk for HA-DVT, pneumonia, and tissue pressure injuries.
- HA-complications penalize hospitals with extended LOS and added unreimbursed treatments costing hospitals significant dollars.
- The nursing team is reluctant to discharge high-risk patients early since hospitals do not provide SCDs for use during home recovery.
- A delay in discharging a patient costs hospitals upwards of $2,000.
- SCDs do not support At-Home DVT Prevention and a readmission due to DVT may cost hospitals as much as $18,681.
- CMS’s Never Event penalizes hospitals financially when self-reporting hospital data shows DVT rate above the baseline. Combining low patient compliance (<50%) and a failure to provide an At-Home DVT Program increases the DVT rates and further exposes hospitals to Medicare’s Never Event penalties.
- Nurses are frustrated with the amount of unproductive time spent removing and reapplying SCD limb sleeves with every bed transfer.
Fact: Those inexpensive SCD limb sleeves are failing hospitals, nurses, and patients in reducing DVT and are costing hospitals millions each year.
Are YOU open to a new, transformational device that improves patient compliance 85%, reduces the risk for DVT 70%, and saves hospitals significant dollars?
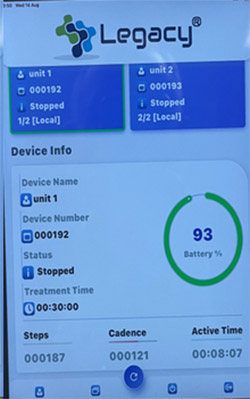
Legacy® IPC is a wearable system designed to promote mobility, monitor and record device performance and patient activity including compliance, steps, cadence, and overall patient activity. Data from the Legacy® App helps nurses when considering early discharges.
Legacy® IPC Device – Promotes Ambulation
- Weighs 5-ounces
- Promotes compliance 85%
- Reduces risk for DVT 70%
- Operates in total silence
- Improves nurse productivity
- Promotes early discharges
- Supports At-home DVT
- Prevents HA-complications
- Reusable with a one-year warranty
- Proven to significantly reduce cost

The Legacy® IPC System represents transformational technology in preventing DVT beginning on day one and until patients are fully ambulatory.
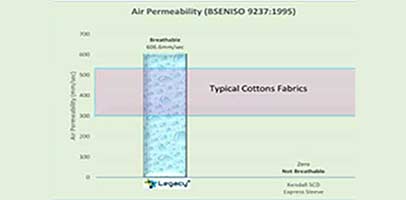
Legacy®Comfort Sleeves
- One-size-fits-all
- Lightweight only 5-ounces
- Soft, breathable fabric
- Conforming fabric
- Prevents slippage during ambulation
- Comfortable to wear for extended hours


Legacy® Monitoring App System improves nurse efficiency and communications with patients.
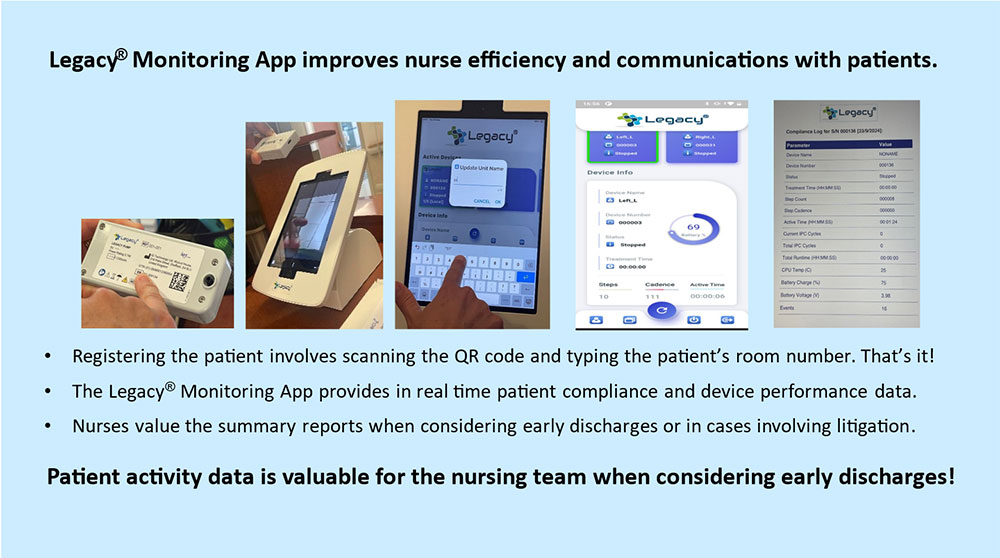
Legacy® Monitoring APP Station
- Bluetooth/W-Fi
- Device performance
- Monitors and tracks Patient Compliance, Steps, Cadence, and Overall Patient Activity
- Data promotes early discharges
- Data retrieval helps in cases involving litigation
- Geolocation tracks device throughout hospital stay
Legacy® Charging Hub
- Charges 20 units at a time
- Fully charged in 3 hours
- Push in docking connection
- Organized charging system
- Compact – 12” x 4”
- Reduces room clutter from plug-ins
- Safety – Reduces leads and trip hazards

The Legacy® IPC is designed to improve the level of care, patient compliance, nurse efficiency, early discharges, reduce HA-DVT, pneumonia, and tissue pressure injuries, along with saving hospitals significant dollars.
1. Legacy®IPC promotes ambulation which improves deep breathing, the clearing of mucus, and reduces the risk for developing HA-pneumonia. Frequent ambulation reduces tissue pressure injuries.
2. Legacy® IPC supports I Cough and ERAS programs.


3. Legacy’s transformational pump weighs 5-ounces, delivers compression every minute for 15 seconds at 45mmHg, and mobilizes venous volume flow equal to bulky SCDs weighing 8 pounds.

4. Legacy’s patented pump operates below 57 dbA, an inaudible level, making it the only device to operate in total silence, which promotes quality rest.
5. The open-cell fabric of the Legacy ® Comfort Sleeves is soft, lightweight, and breathable, which further promotes ambulation, wear time, and patient compliance.
6. The one-size-fits-all Legacy® Comfort Sleeves eliminate inventory issues and the removing and re-applying limb sleeves. Nurses appreciate the improved productivity.


7. The Legacy® Monitoring APP with Bluetooth/Wi-Fi allows nurses to monitor device performance and patient compliance in real time throughout hospital stay.
Traffic Light System
- On – Green
- Blockage – Red
- Low Battery – Amber
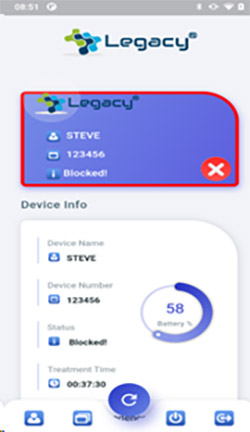
- If an event occurs, the Legacy® App immediately moves the patient information to the top line and the border color goes from green to red signifying an issue.
- Monitoring enhances patient care, leading to positive outcomes.
- Monitoring patient compliance, steps, cadence, and overall patient activity helps discharge planners make informed decisions leading to early discharges that helps save hospitals significant dollars.
The Legacy® APP also provides Geolocation which helps find misplaced devices.
8. Legacy® IPC device and bladder system are reusable. The Legacy® device has a one-year warranty. The single patient Legacy® Comfort Sleeves are purchased as a replacement item


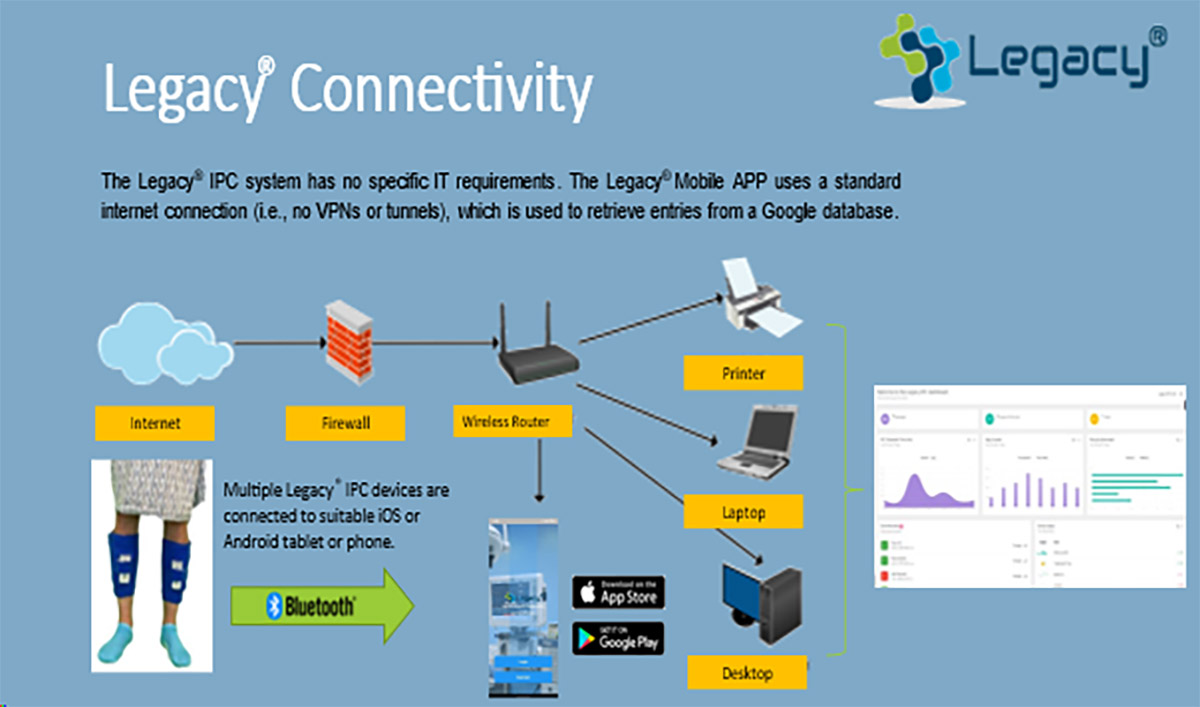
Legacy® APP has no specific IT requirements. Our App uses a standard internet connection
Why use SCDs that fail to …
- Promote ambulation leading to higher DVT rates.
- Promote high patient compliance.
- Reduce noise causing sleep disturbance and discomfort.
- Reduce the risk of HA-DVT, pneumonia, and tissue pressure injuries.
- Promote early discharges that further penalize hospitals financially.
- Support At-Home DVT Prevention Program leading to readmissions.
- Reduce excessive nurse time spent with SCD sleeves.
The transformational technology of the Legacy® IPC makes the case for hospitals to embrace the Legacy® DVT Prevention System as “standard of care” for preventing DVT for all high-risk patients.

