
Occurrence of DVT:
The rate of DVT with active adults is 0.4%. Hospitalize those same individuals and the rate increases to 5% and higher for patients undergoing joint replacement surgery.
Being bed bound plays a major role in the development of DVT.




Bed Stay Increases Risk for DVT, Pneumonia, and Tissue Breakdown Due to Calf Muscle Pump Failure.
Every admission is at risk for developing DVT due to being bed bound during hospital stay. Immobility prevents ankle flexion which leads to calf muscle pump failure and a 47% reduction in venous outflow back to the heart. Studies show sluggish venous blood flow is the culprit of over 60% of clots developing behind the valve cusps of the deep leg veins.
Reduced blood flow due to calf muscle pump failure increases viscosity of mucus and the risk for developing pneumonia. It also impacts the ability of tissue to regulate temperature and metabolic needs which contributes to tissue breakdown.
A Real Need for a Device That Improves Blood Flow and Promotes Frequent Ambulation.
SCDs Fail Patients, Nurses, and Hospitals.



Sequential compression device (SCD) technology was developed in the 1980’s to treat lymphedema. This same technology was adopted to help prevent DVT.
Compliance with SCDs is below 40% due to patients finding limb sleeves too hot, pumps noisy, and a general frustration in feeling constrained with limb sleeves, tubing, hoses, and power cords.
Nurses are frustrated with the amount of unproductive time spent removing and reapplying SCD limb sleeves whenever patients visit the restroom. Studies show the average number of restroom visits is six, which cost hospitals approximately $30.00 per day per patient in non-productive nursing time.
SCD technology does not promote ambulation which further increases the risk for Veterans developing DVT, pneumonia, and/or tissue breakdown.
Hospital policy does not provide SCDs to high-risk patients for use during home recovery which leads to an increase in readmissions due to DVT. This same policy discourages nurses/physicians from considering early discharges which further exposes patients to hospital acquired complications.
Studies show 60% of VTE cases occur after leaving the hospital.
Kendall SCD™ 700 Compression System and Kendall SCD™ Express Sleeves are trademarks of the Kendall International, Inc.
Arjo Huntleigh Flowtron® Express DVT System and Flowtron Compression Sleeves are register marks of the Arjo Company.
Why Use Devices That Consistently Fail to Meet the Needs of Patients, Nurses, and Hospitals?
Legacy® IPC was Designed and Engineered to Meet the Needs of Patients, Nurses, and Hospitals.
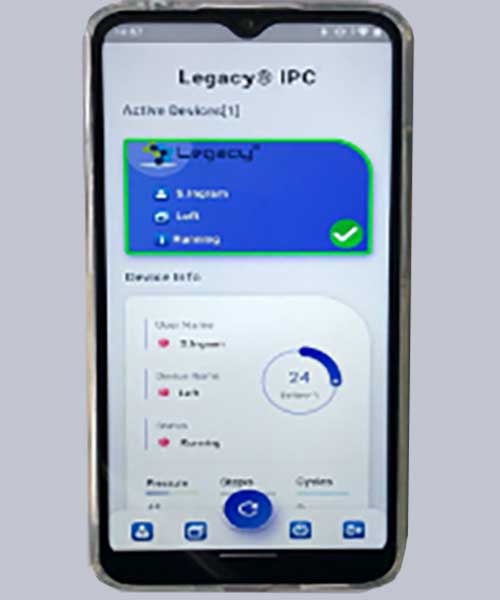
Blocked Pump Alert:
If the device detects a blockage in the air system, then Legacy’s Mobile APP will show a “Blocked” alert. This will remain until the blockage is resolved and the device is running correctly.
Legacy Mobile APP Features:
- Leak alert
- Blockage alert
- Low battery alert
- STEPS counter
- CADENCE counter
- OVERALL ACTIVITY
- Cycle counter
- Battery monitor
- Geo location



Legacy utilizes advanced technology which mobilizes the same venous volume and velocity as SCD units, yet weighs only 70 grams, is totally silent, promotes frequent ambulation, promotes patient and nurse compliance above 85%, and reduces DVT by 70%.
Legacy alerts any changes in operation with the LED flashing green (operating), amber (low battery), or red (fault) with audible alarm to alert staff.
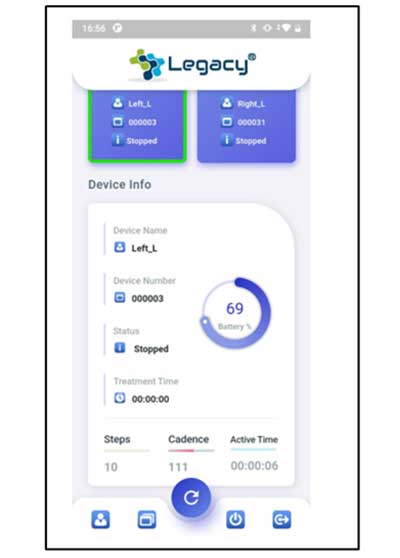
Legacy’s MOBILE APP, along with Bluetooth enables staff to monitor device operation and compliance in real time during hospital stay and throughout home recovery for high-risk patients.
Legacy MOBILE APP monitors STEPS, CADENCE, and ACTIVITY, which is valuable information for nursing in monitoring compliance and certainly helps when considering early discharge.
The Advanced Portable Legacy® IPC Technology Addresses the Clinical, Functional, and Financial Goals Involved in Reducing DVT.
Legacy® IPC Promotes Wear Time and Reduces HA-Complications

Legacy travels with patients while undergoing various procedures including X-ray, CT, and Nuclear Medicine.
Prior to an MRI procedure, the staff simply removes the Legacy devices from the sleeve holsters. After the procedure, the devices are reinserted into each holster. This step takes all of 10 seconds!
Legacy is engineered to increase wear time and compliance by more than 85% and reduce DVT by 70%.
Legacy improves venous, arterial, and lymphatic blood flow which helps rid the body of pathogens and reduces the risk of pneumonia. In addition, improved blood flow helps tissue better regulate temperature and metabolic needs which helps reduce tissue breakdown.
Studies show frequent ambulation further helps prevent the development of DVT, pneumonia, and/or tissue breakdown, which saves hospitals millions and minimizes exposure to CMS’s Never Events Policy.
There are no hoses or tubes to rub against the skin leading to tissue injury.
High compliance and product familiarization promotes early discharge with patients wearing the Legacy® IPC upon leaving the hospital for home recovery.
Legacy® IPC Improves Nurse Productivity, Promotes Ambulation, and Saves Hospitals Millions.

Arjo Flowtron DVT System and Flowtron Sleeves are registered with Arjo Huntleigh

Legacy eliminates unproductive nurse time involved with removing and reapplying SCD limb sleeves, reduces job burn-out, and saves hospitals significant dollars per patient per day.
Legacy improves quality nurse time, quality of care, and generates positive outcomes.
Legacy promotes independence for patients to visit the restroom when needed.
Legacy promotes frequent ambulation which reduces the risk for DVT, HA-pneumonia and tissue breakdown.
High patient compliance, along with product familiarity, promotes early discharges which saves hospitals millions.
Legacy’s MOBILE APP monitors operation, compliance, along with recording STEPS, CADENCE, and ACTIVITY. This data further helps nurses assess patient’s health status and consideration for early discharge.
Legacy’s APP Further Improves Nurse Productivity.
Legacy® Comfort Sleeves are Comfortable, Promote Wear Time, and Reduce DVT.

The National Surgical Quality Improvement Program found portable device technology reduces DVT from a baseline of 4% to 0.8% based on patients wearing the device for at least 18 hours per day.
Patients find Legacy’s Comfort Sleeves extremely soft, lightweight, breathable, and comfortable due to the unique open cell stretchable fabric. Every aspect promotes wear time, compliance above 85%, and DVT reduction by 70%.
Legacy® Comfort Sleeves incorporate a secure 3-point fastening system designed to prevent sleeves from slipping.
The one-size Comfort Sleeves enhance storage space and improve availability.
Legacy operates continuously for 24 hours on a 3-hour charge.
Designed for the device to be positioned on the shin further promotes comfort while sleeping.
Legacy delivers dynamic compression of 45mmHg for 15 seconds every minute.
Legacy® IPC has a one-year warranty.
Reusability of the Legacy® IPC Pumps Significantly Reduces Cost.
For your consideration:
- Would reducing your current DVT rate by 60-70% address your clinical goals?
- Would reducing HA-pneumonia and/or tissue injury further address your clinical goals?
- Would increasing your rate of early discharges help reduce patients being exposed to HA-complications?
- What dollar value would you place on improving nurse productivity and job satisfaction?
- Legacy® IPC offers your hospital system the following benefits:
- Improve patient/nurse compliance by over 80%.
- Reduce DVT by 70%.
- Extend DVT prevention therapy to high-risk patients throughout home recovery (7-14 days).
- Save approximately $30.00 per patient per day in improved nurse productivity.
- Increase early discharges, improve bed management, and reduce exposure to hospital complications.
- Prevent readmissions or extended L.O.S. due to DVT, pneumonia, and tissue injury cases.
The cost to use the Legacy® IPC System is ZERO when considering our technology improves patient and nurse compliance by over 80%, reduces the rate of DVT by 70%, improves nurse productivity by an hour a day, promotes earlier discharges in at least 30% of inpatients, reduces hospital acquired complications due to shorter stays, and extends DVT prevention therapy throughout home recovery for your high-risk patients.
To schedule a Legacy® IPC product presentation, please email john@vasocare.com or phone 225-978-6696.
VasoCARE looks forward to working with you and your Team.
Thank you,
John Berges
President

